Clinical outcome after SVR: Veterans Affairs
Backus L, AASLD 2017, Abs. 78
Design
- Observational cohort (Veterans Affairs Registry)
- All patients treated with DAA, separated in 2 groups
- No advanced liver disease: FIB-4 = 3.25 and absence of cirrhosis, liver decompensation, HCC or liver transplant
- Advanced liver disease: FIB-4 > 3.25
- Overall all-cause mortality and incident HCC: rate per 100 patient-years of follow-up
- 1 year-mortality and incident HCC after end of treatment (censoring date May 31, 2016)
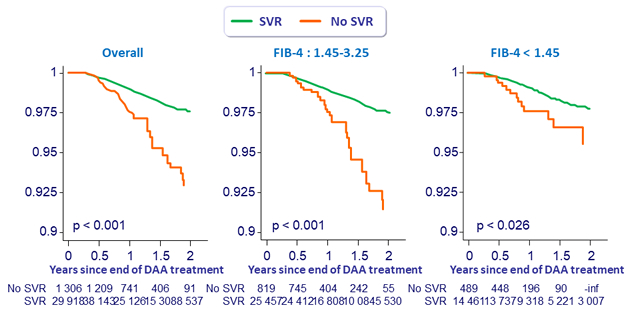
- Kaplan-Meier curves of survival and of HCC-free survival by SVR compared with log-rank tests
- Mortality and incident HCC rates compared with Exact Poisson test
- One-year mortality and HCC rates compared with proportion tests
- Cox proportional hazard models to identify predictors of mortality and the impact of SVR
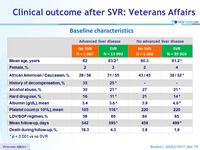
Baseline characteristics
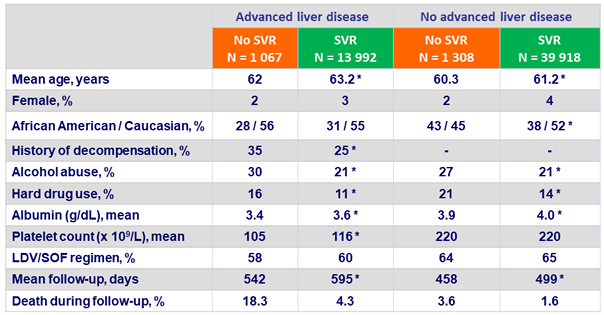
* p < 0.001 vs no SVR
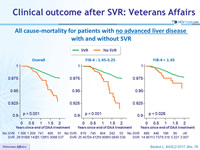
All cause-mortality for patients with no advanced liver disease with and without SVR
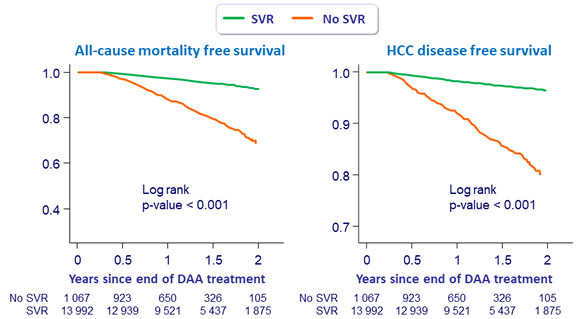
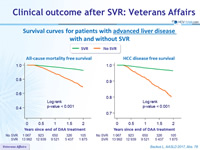
Survival curves for patients with advanced liver disease with and without SVR
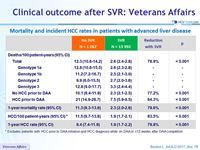
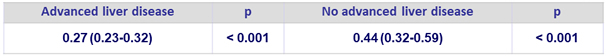
Mortality and incident HCC rates in patients with advanced liver disease
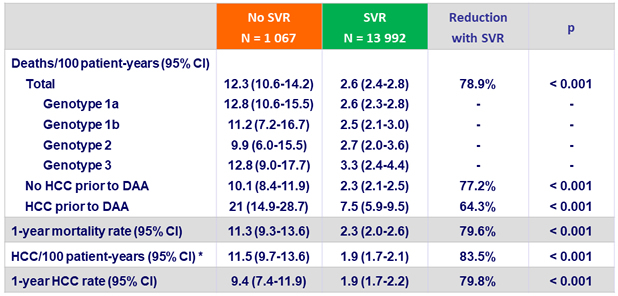
* Excludes patients with HCC prior to DAA initiation and HCC diagnosis while on DAA or =12 weeks after DAA completion
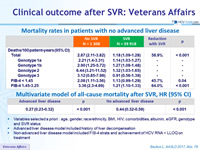
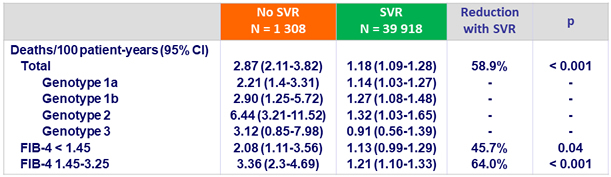
Mortality rates in patients with no advanced liver disease
Multivariate model of all-cause mortality after SVR, HR (95% CI)
- Variables selected a priori : age, gender, race/ethnicity, BMI, HIV, comorbidities, albumin, eGFR, genotype and SVR status
- Advanced liver disease model included history of liver decompensation
- Non-advanced liver disease model included FIB-4 strata and achievement of HCV RNA < LLOQ on treatment
Conclusions
- SVR after DAA was associated with
- Significant lower all-cause mortality, regardless of genotype
- Reduction of risk of 78.9% in patients with advanced chronic liver disease
- Reduction of risk of 58.9% in patients with non-advanced chronic liver disease
- Significant lower incidence of HCC
- Reduction of risk of 83.5%
- Significant lower all-cause mortality, regardless of genotype